Crohn’s Disease and Ulcerative Colitis
What are Crohn’s Disease and Ulcerative Colitis?
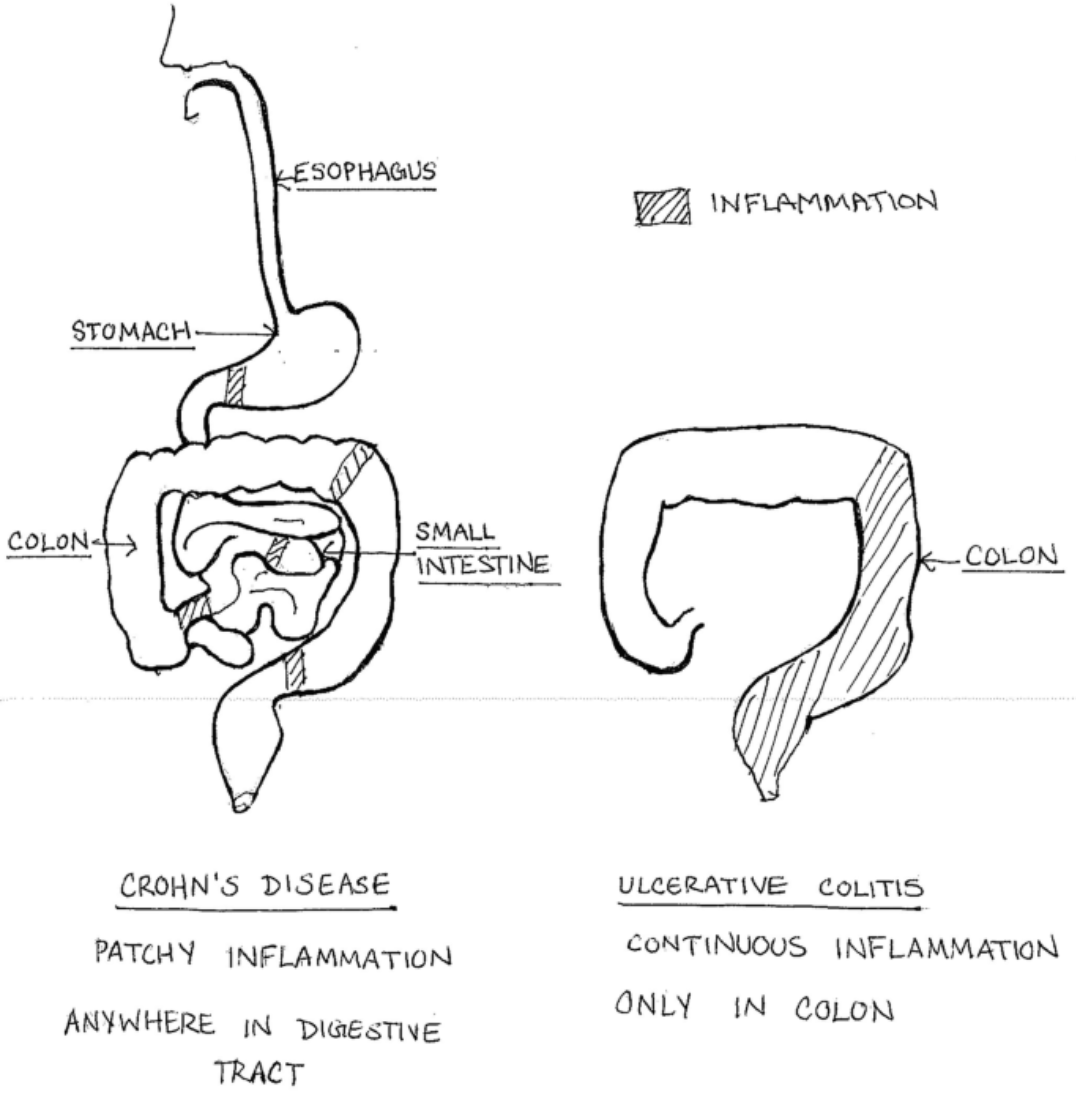
Crohn's Disease and Ulcerative Colitis are chronic inflammatory conditions of the gastrointestinal (GI) tract, collectively known as Inflammatory Bowel Disease (IBD). While both conditions share similarities, they have distinct characteristics that differentiate them.
Crohn's Disease can affect any part of the GI tract, from the mouth to the anus, but it most commonly impacts the end of the small intestine (ileum) and the beginning of the colon. This condition is characterised by patchy areas of inflammation, which can penetrate deeply into the layers of the bowel wall, leading to a variety of complications including strictures, fistulas, and abscesses.
Ulcerative Colitis, on the other hand, is limited to the colon and rectum. It typically starts in the rectum and can extend in a continuous manner to other parts of the colon. The inflammation in Ulcerative Colitis is usually confined to the innermost lining of the colon, causing ulcers or sores.
Pathophysiology and Symptoms
Both conditions result from an inappropriate immune response where the immune system attacks the body's own tissues, leading to inflammation. This autoimmune response is believed to be triggered by a combination of genetic predisposition and environmental factors.
Symptoms of Crohn's Disease:
Abdominal pain and cramping
Chronic diarrhea
Weight loss and malnutrition
Fatigue
Fever
Blood in the stool (in some cases)
Symptoms of Ulcerative Colitis:
Diarrhea, often with blood or pus
Abdominal pain and cramping
Urgency to defecate
Weight loss
Fatigue
Rectal pain and bleeding
Nutritional Deficiencies in IBD
Patients with Crohn's Disease and Ulcerative Colitis often experience various nutritional deficiencies due to several factors:
Malabsorption: Inflammation of the intestinal mucosa impairs the absorption of nutrients.
Reduced Intake: Symptoms like pain, nausea, and diarrhea can reduce appetite and food intake.
Increased Nutrient Loss: Frequent diarrhea leads to significant loss of electrolytes and nutrients.
Increased Requirements: Chronic inflammation increases the body's demand for certain nutrients.
Common deficiencies include:
Vitamins: Vitamin B12, Vitamin D, Vitamin K, and folic acid
Minerals: Iron, calcium, magnesium, and zinc
Macronutrients: Protein-energy malnutrition due to poor intake and increased metabolic demands
Nutritional Support and Dietary Plans
Implementing a tailored dietary plan can play a critical role in managing IBD and improving patient outcomes. Here are key dietary strategies and nutrients to focus on:
Anti-inflammatory Diet:
Omega-3 Fatty Acids: Found in fish oil and flaxseeds, omega-3s have anti-inflammatory properties.
Antioxidants: Foods rich in vitamins A, C, and E, such as berries, spinach, and nuts, help combat oxidative stress.
Probiotics and Prebiotics:
Probiotics: These beneficial bacteria, found in yogurt and fermented foods, can help restore gut flora balance.
Prebiotics: Fiber-rich foods like garlic, onions, and bananas support the growth of healthy bacteria.
Micronutrient Supplementation:
Vitamin D: Crucial for bone health and immune function; supplementation might be necessary due to malabsorption.
Iron: Essential for preventing anemia; consider iron-rich foods or supplements.
Calcium and Magnesium: Important for bone health, especially if corticosteroids are used.
Elimination Diets:
Identifying and eliminating foods that trigger symptoms can help reduce inflammation. Common triggers include dairy, gluten, and high-fiber foods during flare-ups.
Hydration:
Ensuring adequate fluid intake is vital, particularly for those experiencing chronic diarrhea.
Conclusion
Understanding the complexities of Crohn's Disease and Ulcerative Colitis is essential for effective management. While medical treatment is crucial, addressing nutritional deficiencies and implementing targeted dietary strategies can significantly support health and wellness. By focusing on anti-inflammatory foods, probiotics, and key nutrient supplementation, individuals with IBD can optimise their nutritional status and improve their quality of life.
If you or a loved one are dealing with Crohn’s Disease or Ulcerative Colitis and would like to explore a personalised nutritional plan, I am here to help. As a clinical nutritionist, I can provide tailored advice and support to meet your specific needs. Book a consultation with me to start your journey towards better health and well-being.